Historic Korean War Photo – Private Frank Hardy
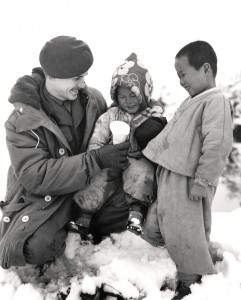
Private Frank Hardy hands a snow cone to a Korean girl. BILL OLSON, LIBRARY AND ARCHIVES CANADA—PA146869
Private Frank Hardy hands a snow cone to a Korean girl. BILL OLSON, LIBRARY AND ARCHIVES CANADA—PA146869

Korean children carrying heavy loads in fan-shaped baskets share a moment with Private Dick Price. BILL OLSON, LIBRARY AND ARCHIVES CANADA—PA184959
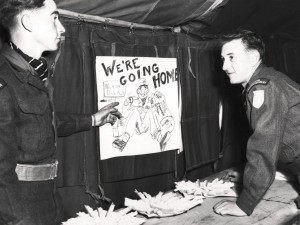
A poster celebrates the start of a homeward-bound trip for some soldiers. MILTON HUNT, LIBRARY AND ARCHIVES CANADA—PA128828

Canadian soldiers hold Chinese propaganda signs recovered in no man’s land. NATIONAL DEFENCE

Signal equipment is checked prior to a night patrol by members of the Royal Canadian Regiment, June 1952. PAUL TOMELIN, LIBRARY AND ARCHIVES CANADA—PA129740

Canadian war artist Ted Zuber’s painting Incoming depicts soldiers of B Company, Royal Canadian Regiment reacting to an enemy artillery attack, October 1952. TED ZUBER,



Get the latest stories on military history, veterans issues and Canadian Armed Forces delivered to your inbox. PLUS receive ReaderPerks discounts!

| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |



Free e-book
An informative primer on Canada’s crucial role in the Normandy landing, June 6, 1944.